Abstract

Introduction: Daratumumab (DARA) is a human IgGκ mAb targeting CD38 with both direct on-tumor and immunomodulatory mechanisms of action, and has been approved as monotherapy for RRMM and in combination with standard of care (SOC) regimens for RRMM and newly diagnosed MM (NDMM). Across three phase 3 DARA studies in RRMM and NDMM, DARA plus SOC reduced the risk of progression or death by ≥50%, enabled a doubling of CR rates, and elicited a ≥3-fold increase in MRD-negative rates. Among MRD-negative RRMM pts, pts treated with D-Rd or D-Vd rapidly achieved MRD negativity and demonstrated prolonged progression-free survival (PFS) vs MRD-positive pts (Avet-Loiseau H, et al. ASH 2016. Abstract 246). MRD assessment is being investigated as a potential surrogate for established endpoints such as overall survival (OS). When measured sequentially, sustained MRD-negativity provides an index of deep clinical responses that may provide a more robust assessment of disease control (Kumar S, et al. Lancet Oncol 2016. 17[8]:e328-e346). Here, we evaluate sustained MRD negativity with DARA plus SOC regimens and its association with PFS/OS outcomes in RRMM.
Methods: Eligible pts in POLLUX and CASTOR received ≥1 prior line of therapy and were randomized (1:1) to receive SOC treatment regimens ± DARA. Pts in the POLLUX study were given lenalidomide (25 mg PO) on Days 1-21 and dexamethasone (40 mg) once per week in each 28-day cycle ± DARA (16 mg/kg IV) given weekly for Cycles 1-2, Q2W for Cycles 3-6, and Q4W thereafter. CASTOR pts received 8 cycles (21 d/cycle) of bortezomib (1.3 mg/m2 SC) on Days 1, 4, 8, and 11 and dexamethasone (20 mg) on Days 1, 2, 4, 5, 8, 9, 11, and 12 ± DARA (16 mg/kg IV) given weekly for Cycles 1-3, Q3W for Cycles 4-8, and Q4W thereafter.
MRD was assessed at the time of suspected CR and at 3 and 6 months following confirmed CR in POLLUX, and at time of suspected CR and 6 and 12 months following the first treatment dose in CASTOR. Additional MRD evaluation was required in both studies every 12 months post-CR. MRD was assessed via next generation sequencing using the clonoSEQ® assay V2.0 (Adaptive Biotechnologies, Seattle, WA). Sustained MRD negativity was defined as the maintenance of MRD negativity in the bone marrow confirmed ≥6 or ≥12 months apart and was evaluated in the intent-to-treat (ITT) population. Sustained MRD negativity was also evaluated among ≥CR pts to account for different sustained MRD negativity rates between treatment arms.
Results: A total of 569 (D-Rd, n = 286; Rd, n = 283) pts in POLLUX and 498 pts (D-Vd, n = 251; Vd, n = 247) in CASTOR were randomized; median (range) number of prior lines received was 1 (1-11) and 2 (1-10), respectively. Median duration of follow up was 39.5 months in POLLUX and 31.3 months in CASTOR for this analysis.
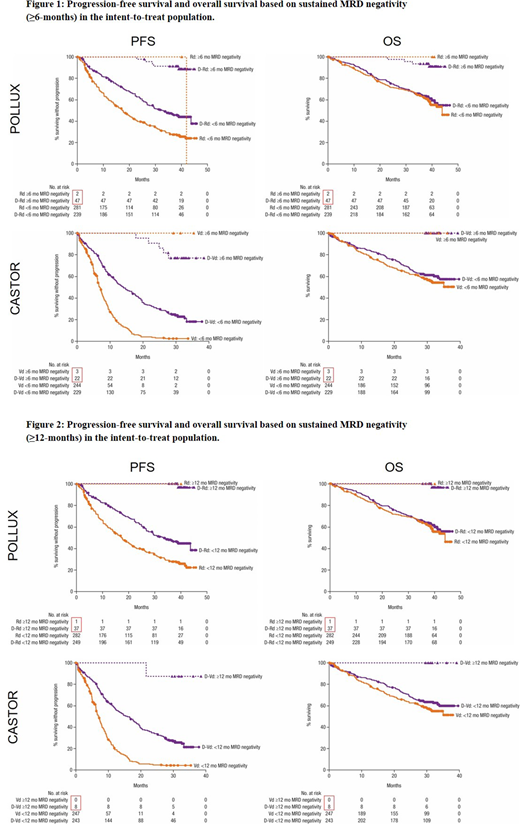
Using the ≥6-month sustained MRD cutoff, a significantly higher proportion of pts achieved sustained MRD negativity for ≥6 months when treated with D-Rd vs Rd (16% vs 0.7%; P <0.0001) and D-Vd vs Vd (9% vs 1%; P = 0.0001) among the ITT population. Among ≥CR pts, the proportion of pts with sustained MRD negativity remained higher for pts treated with D-Rd vs Rd (30% vs 3%; P <0.0001) and D-Vd vs Vd (31% vs 13%; P = 0.11). While significantly fewer pts receiving SOC alone achieved sustained MRD negativity, sustained MRD negativity was associated with longer PFS and OS in all treatment arms vs pts without sustained MRD negativity in the ITT population (Figure 1).
For the ≥12-month sustained MRD cutoff, more pts achieved sustained MRD negativity when receiving D-Rd vs Rd (13% vs 0.4%; P <0.0001) and D-Vd vs Vd (3% vs 0%; P = 0.0074) in the ITT population. Similar trends were observed for sustained MRD negativity rates among ≥CR pts treated with D-Rd vs Rd (24% vs 2%; P <0.0001) and D-Vd vs Vd (11% vs 0%; P = 0.19). Achievement of sustained MRD negativity for ≥12 months also consistently demonstrated longer PFS and OS for DARA-containing regimens vs those without sustained MRD negativity in the ITT population (Figure 2).
Additional analyses, including an analysis of baseline pt characteristics for pts with sustained MRD negativity, will be presented at the meeting.
Conclusions: DARA combinations with SOC regimens enable a significantly higher proportion of pts to achieve deep and durable responses of ≥CR and MRD negativity at 10-5. Importantly, the ability to reach durable MRD negativity is associated with prolonged survival, suggesting that achieving durable MRD negativity should be a treatment goal for RRMM pts.
San-Miguel:Sanofi: Honoraria; Novartis: Honoraria; BMS: Honoraria; Amgen: Honoraria; Celgene: Honoraria; Janssen: Honoraria; Roche: Honoraria. Casneuf:Janssen Research & Development: Employment. Iida:Chugai: Research Funding; Astellas: Research Funding; Bristol Myers Squibb: Honoraria, Research Funding; Kyowa-Hakko Kirin: Research Funding; MSD: Research Funding; Gilead: Research Funding; Toyama Chemical: Research Funding; Teijin Pharma: Research Funding; Sanofi: Consultancy; Novartis: Honoraria, Research Funding; Celgene: Honoraria, Research Funding; Janssen: Consultancy, Honoraria, Research Funding; Ono: Consultancy, Honoraria, Research Funding; Takeda: Consultancy, Honoraria, Research Funding. Lonial:Amgen: Research Funding. Usmani:Amgen, BMS, Celgene, Janssen, Merck, Pharmacyclics,Sanofi, Seattle Genetics, Takeda: Research Funding; Abbvie, Amgen, Celgene, Genmab, Merck, MundiPharma, Janssen, Seattle Genetics: Consultancy. Spencer:Celgene: Honoraria, Research Funding, Speakers Bureau; Janssen-Cilag: Honoraria, Research Funding, Speakers Bureau; Amgen: Honoraria, Research Funding; BMS: Research Funding; Takeda: Honoraria, Research Funding, Speakers Bureau; STA: Honoraria. Moreau:Takeda: Honoraria, Membership on an entity's Board of Directors or advisory committees; Amgen: Honoraria, Membership on an entity's Board of Directors or advisory committees; Celgene: Honoraria, Membership on an entity's Board of Directors or advisory committees; Abbvie: Honoraria, Membership on an entity's Board of Directors or advisory committees; Janssen: Honoraria, Membership on an entity's Board of Directors or advisory committees. Plesner:Celgene: Other: Independent Response Assessment Comittee; Janssen: Consultancy. Weisel:Amgen, BMS, Celgene, Janssen, Juno, Sanofi, and Takeda: Consultancy, Membership on an entity's Board of Directors or advisory committees; Amgen, BMS, Celgene, Janssen, and Takeda: Honoraria; Amgen, Celgene, Janssen, and Sanofi: Research Funding. Ukropec:Janssen Scientific Affairs, LLC: Employment. Okonkwo:Janssen Research & Development, LLC: Employment. Trivedi:Janssen Research & Development, LLC: Employment. Velas:Janssen Research & Development, LLC: Employment. Qin:Janssen Research & Development, LLC: Employment. Qi:Janssen Research & Development, LLC: Employment. Chiu:Janssen Research & Development, LLC: Employment. Bahlis:Amgen: Consultancy, Honoraria, Research Funding; Celgene: Consultancy, Honoraria, Research Funding; Janssen: Consultancy, Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal